Adderall ranks as the fifteenth most commonly prescribed medication in the United States, with more than 32 million prescriptions issued in 2023 alone. However, despite its widespread use, many patients still wonder what Adderall actually is and how it affects the body. As a Schedule II controlled substance, this powerful stimulant medication requires careful consideration and proper understanding.
In fact, the misuse of stimulant medications like Adderall has been growing over the past two decades, with approximately 5.1 million people aged 12 or older misusing prescription stimulants in 2020. Consequently, knowing how long Adderall lasts (typically 10-13 hours in adults) and recognizing potential adderall side effects becomes crucial for anyone using this medication. Throughout this guide, we’ll explore everything you need to know about Adderall—from its composition and uses to safety concerns and alternatives like Ritalin.
What is Adderall and how does it work?
Prescribed to millions of patients annually, Adderall belongs to a class of central nervous system (CNS) stimulants used primarily to treat attention deficit hyperactivity disorder (ADHD) and narcolepsy. Understanding this medication’s composition and mechanism of action can help patients make informed decisions about their treatment.
Adderall generic name and composition
The generic name for Adderall is “mixed amphetamine salts” or “dextroamphetamine-amphetamine.” This medication contains a specific combination of amphetamine salts blended in a particular ratio. Specifically, Adderall contains four different amphetamine salts: dextroamphetamine saccharate, amphetamine aspartate, dextroamphetamine sulfate, and amphetamine sulfate. These salts are combined to create a 3:1 ratio of dextroamphetamine to levoamphetamine.
This precise combination is significant because each component contributes differently to the medication’s effects. Dextroamphetamine (d-amphetamine) is approximately three to four times more potent as a central nervous system stimulant than levoamphetamine (l-amphetamine) and acts primarily on dopamine. Meanwhile, levoamphetamine produces stronger cardiovascular and peripheral effects and acts primarily on norepinephrine at lower doses. Together, these components create Adderall’s unique therapeutic profile.
Immediate-release vs extended-release (Adderall XR)
Adderall comes in two primary formulations with significant differences in how they’re released into the body:
Immediate-release (IR):
- Available as uncoated tablets
- Effects begin within 45-60 minutes after ingestion
- Peak effect occurs in 2-3 hours
- Duration of action lasts approximately 4-6 hours
- Often requires multiple daily doses (typically morning and afternoon)
Extended-release (Adderall XR):
- Available as capsules filled with coated beads
- Uses a double-bead formulation where half the beads release immediately while the other half dissolve more slowly
- Effects peak about 4-7 hours after ingestion
- Duration of action lasts approximately 8-12 hours
- Typically requires only one morning dose daily
Additionally, a newer extended-release formulation called Mydayis uses a triple-bead system and can last up to 16 hours in individuals 13 years and older.
How Adderall affects the brain
Fundamentally, Adderall works by altering the concentration of certain neurotransmitters—primarily dopamine and norepinephrine—in the brain. As a CNS stimulant, it employs several mechanisms to achieve this effect:
Adderall enters the presynaptic neuron either through diffusion or by using the monoamine transporters (DAT, NET, and SERT). Once inside, it increases neurotransmitter levels through multiple actions:
- It inhibits the vesicular monoamine transporter 2 (VMAT2), preventing neurotransmitters from being stored in vesicles
- It blocks the reuptake of norepinephrine and dopamine into the presynaptic neuron
- It increases the release of these monoamines into the extraneuronal space
- It inhibits monoamine oxidase (MAO), which normally breaks down these neurotransmitters
For individuals with ADHD, who typically have lower baseline levels of dopamine, Adderall brings the brain from a state of overstimulation to a more normal state of stimulation. This helps decrease impulsivity while improving attention and focus.
The medication’s effects on dopamine specifically affect the brain’s reward and pleasure centers, creating feelings of motivation. Meanwhile, the effects on norepinephrine influence attention and response, primarily in the prefrontal cortex of the brain.
Approved medical uses of Adderall
The FDA has officially approved Adderall for treating two specific conditions, though its applications extend beyond these official uses. Understanding precisely what Adderall is used for helps patients recognize when this medication might be appropriate for their symptoms.
Treatment for ADHD
Attention deficit hyperactivity disorder (ADHD) represents the primary approved use for Adderall. Studies show that approximately 75-80% of children with ADHD experience significant improvement in their symptoms when taking this medication. The prevalence of ADHD has increased notably in recent years, rising from 7.8% in 2003 to 9.5% in 2007 among children aged 4-17 years—a 21.8% increase in just four years.
For adults, ADHD affects between 3.5% and 4.5% of the population. Both immediate-release Adderall tablets and extended-release Adderall XR capsules are FDA-approved for treating ADHD in children and adults. The medication works by increasing dopamine levels in the brain, which helps alleviate core ADHD symptoms including hyperactivity, impulsivity, and inattention.
Essentially, Adderall helps patients maintain focus and concentration while reducing hyperactive behaviors. For many individuals with ADHD, this improvement in symptom control translates to better academic performance, enhanced work productivity, and improved social interactions.
Use in narcolepsy
Narcolepsy, a chronic sleep disorder affecting approximately 25 to 50 people out of every 100,000 worldwide, represents the second FDA-approved use for Adderall. This condition causes excessive daytime sleepiness, sleep attacks, and in some cases, sudden muscle weakness (cataplexy).
People with narcolepsy often struggle to stay awake during daytime activities and may fall asleep suddenly in the middle of activities. Adderall oral tablets (immediate-release formulation) are approved to treat this condition, though the extended-release version isn’t typically prescribed for narcolepsy.
Given that narcolepsy stems from the death of brain cells that produce hypocretin (a chemical essential for regulating sleep-wake cycles), Adderall helps by boosting norepinephrine levels to promote wakefulness. For individuals with narcolepsy, taking stimulants like Adderall at the start of the day enhances daytime alertness, which may also improve nighttime sleep quality.
Off-label and less common uses
Apart from FDA-approved applications, physicians sometimes prescribe Adderall “off-label” for conditions that lack formal FDA approval. These uses include:
- Treatment-resistant depression: Although not FDA-approved for this purpose, Adderall has occasionally been prescribed for depression that hasn’t responded to standard treatments. This practice has historical roots—amphetamines were used to treat depression from the 1930s until the 1950s when dedicated antidepressants were discovered.
- Depression with ADHD: First of all, some doctors prescribe Adderall to address depression in individuals who have both ADHD and depression. In such cases, the medication may improve symptoms of both conditions simultaneously.
- Anxiety with ADHD: Furthermore, Adderall is sometimes prescribed off-label for individuals with anxiety, particularly those who have comorbid ADHD and anxiety disorders. Research suggests combining stimulant medications with antidepressants might improve symptoms of both conditions.
- Bipolar disorder: In certain cases, Adderall and other stimulants may be prescribed off-label to treat depressive symptoms in bipolar disorder patients. When used for this purpose, stimulants are typically combined with other bipolar medications rather than used alone.
These off-label applications remain controversial among medical professionals, primarily due to concerns about potential misuse and addiction, alongside limited research supporting these applications compared to FDA-approved uses.
Short-term and long-term effects of Adderall
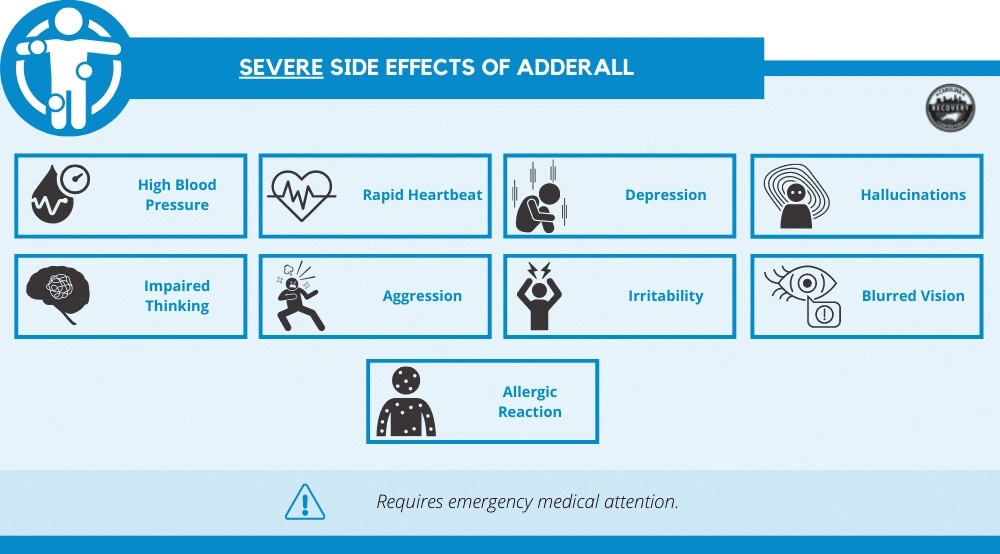
Image Source: Carolina Center for Recovery
Taking Adderall often produces both immediate effects and potential long-term consequences that patients should consider carefully before starting treatment. The medication’s impact varies based on dosage, duration of use, and individual factors such as age and overall health.
Common short-term side effects
Many patients experience transient side effects shortly after beginning Adderall treatment. These typically emerge within the first hour as the medication begins working and may subside as the body adjusts. Common short-term side effects include:
- Anxiety and nervousness
- Dry mouth and stomach discomfort
- Headaches and dizziness
- Reduced appetite and weight loss
- Sleep difficulties and insomnia
- Increased blood pressure and heart rate
- Unusual sense of well-being
Fortunately, many of these side effects diminish as your body adapts to the medication. Nevertheless, approximately one study found children with ADHD were more likely to experience headaches than those without ADHD.
Long-term risks and dependency
With extended use, Adderall may lead to several concerning effects. Most significantly, the medication can become habit-forming as it increases dopamine levels and creates feelings of euphoria. This risk is heightened among individuals taking Adderall without a medical need for it.
Moreover, tolerance typically develops over time, requiring larger quantities to maintain the same therapeutic effect. This phenomenon occurs as the brain adapts to consistent stimulant exposure by altering neurotransmitter function and receptor density.
Studies suggest that prolonged stimulant use might cause changes in brain structure and function, primarily in areas associated with reward, motivation, and executive function. Initially, tolerance appears within the first three years of cumulative use.
Impact on heart and mental health
Cardiovascular concerns represent serious long-term risks. Adderall can raise blood pressure and heart rate, potentially leading to complications for people with preexisting conditions. Recent research found individuals prescribed stimulants were 17% more likely to develop cardiomyopathy (weakened heart muscle) at one year and 57% more likely after eight years compared to non-users.
Regarding mental health, the risk of developing psychosis from Adderall, although low, exists—particularly with high doses. One study showed that among young adults with ADHD receiving prescription stimulants, approximately 1 in 660 patients experienced first-time psychosis. Surprisingly, this risk was twice as high for Adderall users compared to those taking Ritalin.
Adderall withdrawal symptoms
When stopping Adderall, patients typically experience a distinctive pattern of withdrawal symptoms. Initially, during the “crash phase” lasting 1-2 days, individuals often experience:
- Excessive sleepiness or insomnia
- Irritability and mood swings
- Increased appetite
- Mild drug cravings
Subsequently, the withdrawal phase continues for 2-4 weeks with more intense symptoms including depression, stronger cravings, disturbed sleep, and lethargy. Some people recover within 5 days, whereas others may experience symptoms for several months, especially after long-term, high-dose usage.
The withdrawal timeline varies based on whether patients used immediate-release or extended-release formulations. Those taking Adderall XR typically begin withdrawal symptoms later but may experience them for a longer period.
Risks, misuse, and addiction potential
Despite its medical benefits, Adderall misuse has increased on high school and college campuses, with approximately 75% of prescription stimulant abuse occurring in these environments. In essence, understanding the signs of misuse and potential for addiction becomes crucial for anyone prescribed this medication.
Signs of misuse and abuse
Adderall misuse takes various forms, including:
- Taking someone else’s prescription
- Using higher doses than prescribed
- Injecting, snorting, or smoking pills
- Mixing with alcohol or other drugs
- Using it to get high or as a study aid
These behaviors often manifest through telltale signs such as being overly talkative, unusual excitability, social withdrawal, declining personal hygiene, and running out of prescriptions early.
Understanding Adderall addiction
Addiction—officially termed severe substance use disorder—means you cannot control your urge to take the drug. Over time, your brain requires more Adderall to achieve the same effect, a phenomenon known as tolerance.
Signs of addiction typically include:
- Intense cravings for the drug
- Continued use despite negative impacts on relationships and finances
- Taking dangerous risks to obtain or use Adderall
- Anxiety, agitation, or paranoia
Recreational use and legal implications
Primarily, young adults and students misuse Adderall to enhance alertness, improve academic performance, or suppress appetite. Unfortunately, the federal government classifies Adderall as a Schedule II controlled substance—the same category as cocaine—indicating high abuse potential.
Legal consequences for possession without a prescription range from misdemeanors to felonies, with first-time federal offenders facing fines between $1-5 million and up to 20 years imprisonment.
Adderall overdose symptoms
An Adderall overdose, although rare, can be life-threatening. Warning signs include:
- Restlessness and agitation
- Rapid breathing and irregular heartbeat
- Confusion and paranoia
- Hallucinations
- Seizures
- Hyperthermia (body temperature of 106.7°F or higher)
- Chest pain
According to recent data, more than 2% of all drug-related overdose deaths in 2017 involved prescription amphetamines like Adderall. This risk increases substantially when mixing Adderall with other substances, particularly opioids or alcohol.
Interactions, alternatives, and safety tips
Safe management of Adderall treatment requires understanding potential interactions and alternatives. This knowledge becomes even more valuable in today’s healthcare landscape with ongoing medication shortages.
Drug and food interactions
Adderall can interact with numerous medications, primarily other drugs affecting brain chemistry. Combining Adderall with MAOIs (monoamine oxidase inhibitors) is particularly dangerous, potentially causing life-threatening high blood pressure. Patients must wait at least 14 days after stopping MAOIs before starting Adderall.
Food interactions also affect medication efficacy. Foods and beverages high in vitamin C can prevent Adderall absorption when consumed within an hour of taking the medication. Similarly, acid-reducing medications like antacids can increase Adderall absorption, potentially intensifying side effects.
Ritalin vs Adderall: key differences
Both Ritalin (methylphenidate) and Adderall (amphetamine-dextroamphetamine) treat ADHD, yet differ significantly. Ritalin works faster but Adderall remains active longer in the body. Typically, Adderall is approximately twice as potent as Ritalin, with a 7.5mg dose of Adderall producing effects comparable to 17.5mg of Ritalin.
Safe usage and dosage guidelines
For ADHD treatment, physicians typically start children with 2.5-5mg daily, gradually increasing as needed. First doses should be taken upon waking, with additional doses 4-6 hours apart.
What to do during the Adderall shortage
Currently, patients facing shortages might consider calling multiple pharmacies or contacting manufacturers directly. Alternatively, trying different formulations or medications like non-stimulants (atomoxetine, viloxazine) offers viable options.
Conclusion
Understanding Adderall requires a comprehensive view of both its benefits and risks. Throughout this guide, we’ve explored how this powerful medication works by altering brain chemistry, primarily affecting dopamine and norepinephrine levels. While Adderall effectively treats ADHD and narcolepsy for millions of patients, the potential for misuse and addiction cannot be overlooked.
Many patients experience short-term side effects like dry mouth, reduced appetite, and sleep difficulties that typically diminish over time. However, long-term risks deserve careful consideration, particularly regarding cardiovascular health and potential dependency. The likelihood of developing tolerance makes proper medical supervision essential for anyone taking this medication.
Students and young adults should be especially cautious about recreational use. Undoubtedly, the legal consequences of misusing this Schedule II controlled substance can be severe, not to mention the physical and psychological risks involved.
Safety remains paramount when taking Adderall. Drug interactions, particularly with MAOIs and vitamin C-rich foods, can significantly impact how the medication works in your body. Additionally, alternatives like Ritalin might provide better options for some patients, especially during ongoing medication shortages.
The decision to use Adderall should always involve careful consultation with healthcare providers. This medication, when prescribed appropriately and taken as directed, helps many individuals manage their conditions effectively. Nevertheless, the responsibility falls on both prescribers and patients to ensure this powerful stimulant serves its intended purpose without causing harm.
Remember that each person responds differently to medication. Therefore, maintaining open communication with your doctor about any side effects or concerns ensures the safest possible treatment journey. Your well-being ultimately depends on making informed choices about medications like Adderall based on personal health needs balanced against potential risks.
Key Takeaways
Understanding Adderall’s composition, effects, and risks is essential for safe and effective treatment of ADHD and narcolepsy.
• Adderall contains four amphetamine salts that increase dopamine and norepinephrine levels, helping 75-80% of ADHD patients improve focus and reduce hyperactivity.
• Extended-release (XR) formulations last 8-12 hours versus 4-6 hours for immediate-release, allowing once-daily dosing for better medication compliance.
• Long-term use carries cardiovascular risks and addiction potential, with tolerance developing within three years and withdrawal symptoms lasting 2-4 weeks.
• Misuse is common among students (75% of abuse occurs in schools), but possession without prescription is a federal crime with severe legal consequences.
• Drug interactions with MAOIs can be life-threatening, while vitamin C reduces absorption—making medical supervision crucial for safe treatment.
When used appropriately under medical guidance, Adderall provides significant benefits for legitimate medical conditions, but its Schedule II classification reflects serious abuse potential that requires careful monitoring and patient education.
FAQs
Q1. What are the most common side effects of Adderall?
Ans:- Common side effects include dry mouth, reduced appetite, sleep difficulties, and mild cardiovascular effects like increased heart rate and blood pressure. In rare cases, more serious cardiovascular reactions can occur.
Q2. How can I take Adderall safely?
Ans:- Take Adderall exactly as prescribed by your doctor. Be aware of its habit-forming potential and inform your healthcare provider about any history of substance abuse. Avoid combining it with other medications without medical approval, especially MAOIs.
Q3. How does Adderall affect someone without ADHD?
Ans:- In individuals without ADHD, Adderall can overstimulate the brain, potentially leading to restlessness, loss of appetite, and difficulty sleeping. It may create a sense of increased focus, but also carries risks of misuse and addiction.
Q4. What are the potential long-term effects of daily Adderall use?
Ans:- Long-term daily use of Adderall may lead to tolerance, dependency, and potential cardiovascular issues. It can also affect growth in children. Regular medical check-ups are important to monitor for these effects.
Q5. How long does Adderall typically stay in your system?
Ans:- The effects of immediate-release Adderall usually last 4-6 hours, while extended-release formulations can last 8-12 hours. However, the drug can be detectable in urine tests for 2-4 days after the last dose, depending on various factors.